
In an autologous stem cell transplant, the donor and recipient are the same person, meaning the patient receives their own stem cells back as part of the treatment.1
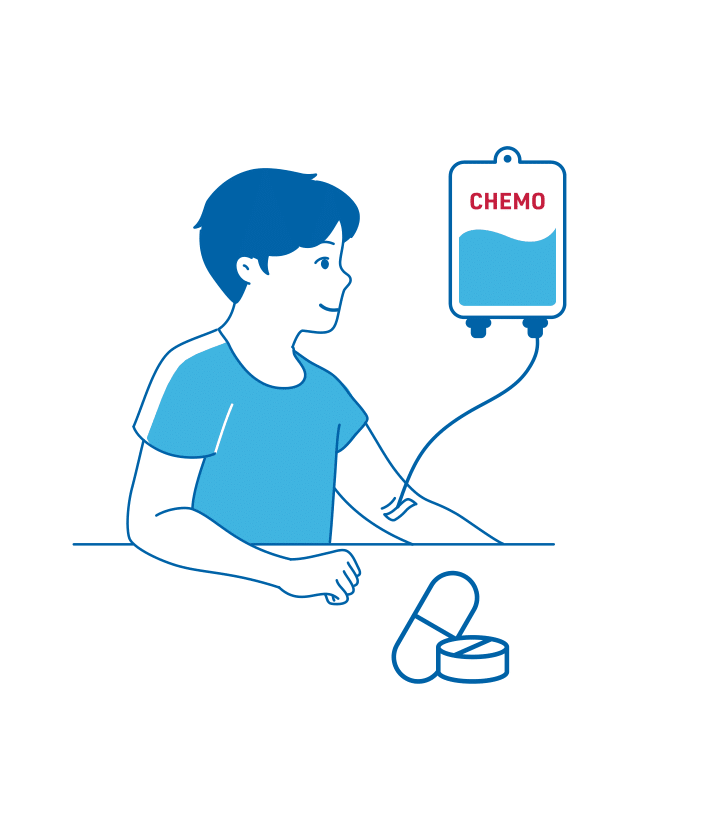
In an autologous stem cell transplant, your own healthy stem cells are collected and stored. You will then receive high-dose chemotherapy, which will not only destroy the lymphoma cells but will also kill the stem cells. After chemotherapy, your stored stem cells are infused back into your body to replace those destroyed by chemotherapy. It can take your bone marrow around 2 to 3 weeks to recover.1,2
An autologous stem cell transplant is used to restore stem cells after high-dose chemotherapy.1
In this type of transplant, the recipient and the donor are the same person.1
1. Salvage treatment (to destroy cancer cells and stimulate stem cell production)
2. Collection of stem cells
3. High-dose chemotherapy (to destroy the remaining lymphoma cells)
4. Transplantation (reinfusion of patient’s own stem cells to restore the blood system)
5. Aftercare – ongoing care and monitoring post-procedure
You may experience side effects from the chemotherapy, or from the stem-cell infusion itself.3,4
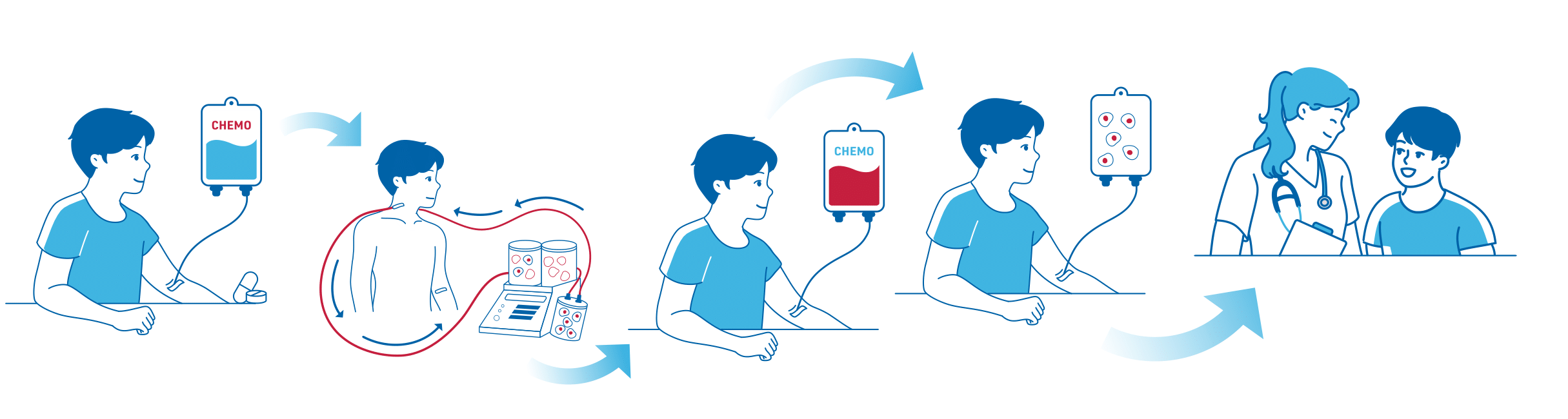
You may need salvage chemotherapy to reduce your tumour burden as much as possible to give you the best chance of responding to a stem cell transplant.3
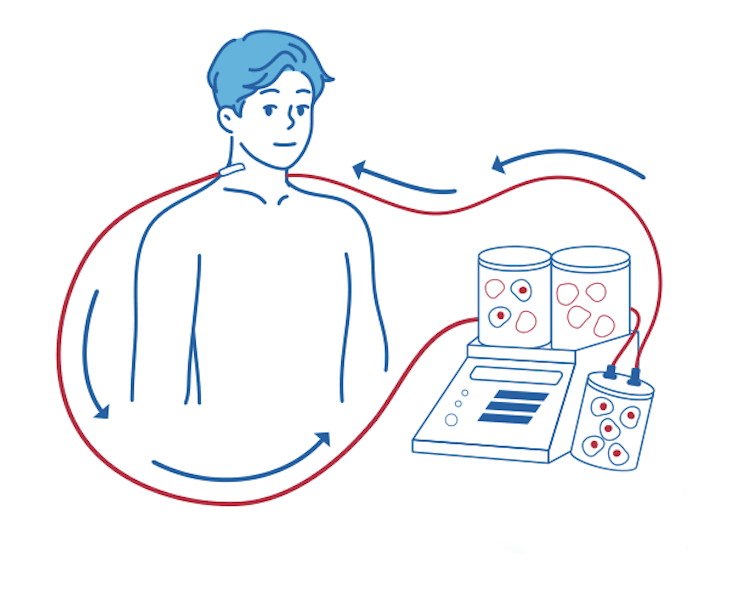
You will also receive treatment to stimulate production of stem cells in your bone marrow, helping the stem cells move into your bloodstream for collection. This process is essential to ensure enough stem cells can be collected for the transplant.3
When you have enough stem cells in your bloodstream, a cell-separator machine filters the stem cells out of the blood – through the process known as apheresis. The rest of the blood cells that are not needed for the transplant are returned to the bloodstream. The process takes a few hours.3
Once enough stem cells have been collected, high-dose chemotherapy is administered again. This intense treatment is designed to destroy as many cancer cells as possible and also clear out the stem cells in your bone marrow to make room for the new ones.3
1–2 days after conditioning (high-dose chemotherapy), the patient’s own blood stem cells are infused back into to the bloodstream.3 These stem cells will develop into healthy blood cells. Some patients can go home straight after their stem cell transplant, particularly if it is an autologous transplant. Inpatient stays are only required if complications arise.3,4

The period post-transplant can be particularly stressful as your immune system will be severely weakened and common infections can become serious. It is important to seek medical attention immediately if any symptoms of infections are experienced.3,5

Possible side effects of an autologous stem cell transplant are described below.
High-dose chemotherapy often leads to side effects including oral mucositis (sore mouth), nausea and vomiting as well as issues with the bowels such as diarrhoea, constipation and wind.2
High-dose chemotherapy also reduces the number of white blood cells, which means that the patient is at high risk of infection during this time, as well as red blood cells (anaemia).2 They may also be at increased risk of bruising and bleeding (thrombocytopenia).2
These are some of the more common side effects, but other side effects may also occur.³ However, complications from tissue rejection do not occur in an autologous transplant since the stem cells come from your own body.4
References: